Introduction
The healthcare landscape in the USA continues to evolve at a remarkable pace, driven by rapid advancements in technology and medical research. In 2024, these innovations are playing a pivotal role in shaping patient care, enhancing not only the quality but also the efficiency of healthcare delivery. The importance of these advancements cannot be overstated, as they are instrumental in improving patient outcomes and transforming the overall healthcare experience.
From cutting-edge diagnostic tools to groundbreaking treatments, the USA remains at the forefront of healthcare innovation. The integration of artificial intelligence, telemedicine, and personalized medicine are just a few examples of how technology is revolutionizing the field. These developments are not only making healthcare more accessible but also more precise, ensuring that patients receive the most effective care tailored to their individual needs.
Moreover, these advancements contribute significantly to streamlining healthcare operations, reducing costs, and minimizing the potential for human error. Enhanced data analytics and interoperability of health information systems are empowering healthcare providers with real-time insights, facilitating more informed decision-making and improving coordination of care. This holistic approach to healthcare signifies a shift towards a more efficient and patient-centric model.
As we delve deeper into the specific innovations that are defining patient care in 2024, it is crucial to recognize the collaborative efforts of researchers, healthcare professionals, and policymakers. Their dedication to advancing medical science and technology underscores the commitment to improving the well-being of individuals and communities across the nation. With these ongoing efforts, the USA continues to set a benchmark for healthcare excellence, paving the way for a healthier future.
Telemedicine and Remote Patient Monitoring
The landscape of healthcare in the United States has been significantly transformed by the rapid advancement of telemedicine and remote patient monitoring. These innovations, greatly accelerated by the COVID-19 pandemic, have redefined how patients access medical care, making healthcare services more accessible and efficient. The widespread adoption of telemedicine has minimized the necessity for in-person visits, allowing patients to consult with healthcare providers from the comfort of their homes. This shift has been particularly beneficial for individuals with mobility issues or those residing in remote areas.
Remote patient monitoring (RPM) has emerged as a crucial component of modern healthcare. RPM technologies enable continuous observation of patients with chronic conditions, ensuring timely interventions and better management of diseases such as diabetes, hypertension, and heart failure. Devices like wearable sensors, smartwatches, and mobile health apps collect real-time data on vital signs, which are then transmitted to healthcare providers for analysis. This not only enhances patient outcomes but also reduces the burden on healthcare facilities by preventing hospital readmissions.
Several companies are at the forefront of telemedicine and RPM innovations. Teladoc Health, a leader in virtual healthcare, has expanded its services to include comprehensive remote monitoring solutions. Their platform integrates advanced analytics with patient data to provide personalized care plans. Similarly, Philips Healthcare offers a range of RPM devices designed to monitor various health parameters and deliver actionable insights to clinicians.
The integration of artificial intelligence (AI) and machine learning (ML) in telemedicine platforms is further enhancing the quality of care. AI-driven algorithms can predict potential health issues by analyzing patient data, allowing for proactive interventions. For example, companies like Livongo use AI to provide real-time health recommendations to patients with chronic conditions, improving their quality of life.
The rise of telemedicine and remote patient monitoring represents a paradigm shift in the healthcare industry. By leveraging cutting-edge technologies, these innovations are not only making healthcare more accessible and efficient but also paving the way for a future where continuous, personalized care is the norm.
Artificial Intelligence and Machine Learning in Diagnostics
Artificial Intelligence (AI) and Machine Learning (ML) are revolutionizing the field of diagnostics, offering unprecedented advancements in medical imaging, disease prediction, and personalized treatment plans. These technologies harness vast amounts of data to enhance diagnostic accuracy, streamline processes, and ultimately improve patient outcomes.
In radiology, AI-powered tools like convolutional neural networks (CNNs) are employed to interpret medical images with remarkable precision. These systems can identify anomalies such as tumors, fractures, and other pathologies that might be missed by the human eye. For instance, AI algorithms are now being used to analyze mammograms, significantly improving the early detection rates of breast cancer. These tools not only reduce the workload of radiologists but also enhance diagnostic accuracy.
Pathology is another area benefitting from AI and ML. Digital pathology platforms leverage AI to analyze tissue samples, aiding in the detection and classification of diseases at a cellular level. This technology accelerates the diagnostic process and ensures consistency, which is critical for diseases requiring swift intervention. AI applications in pathology are proving particularly valuable in oncology, where precise and timely diagnoses are crucial.
In the realm of genomics, AI and ML are instrumental in interpreting complex genetic data. By analyzing large genomic datasets, AI can identify genetic predispositions to various diseases, enabling early intervention and personalized treatment plans. For example, AI-driven platforms are being used to predict responses to specific treatments in cancer patients, allowing for more targeted and effective therapies.
Moreover, AI and ML are pivotal in predicting disease outbreaks. By analyzing diverse data sources, including social media, travel patterns, and climate data, these technologies can forecast potential epidemic hotspots, allowing for preemptive measures and resource allocation. This predictive capability is invaluable for global health security, particularly in managing infectious diseases.
Significant AI-powered tools such as IBM Watson for Oncology, Google DeepMind’s health projects, and PathAI are at the forefront of these innovations. Their applications across radiology, pathology, and genomics underscore the transformative potential of AI and ML in modern diagnostics, shaping a future where patient care is more precise, personalized, and proactive.
Genomic Medicine and Personalized Healthcare
Genomic medicine represents a transformative approach in modern healthcare, leveraging the intricacies of our genetic makeup to tailor medical treatments to individual patients. In recent years, the USA has been at the forefront of advancements in this field, spearheading initiatives that aim to decode the human genome and utilize this data for personalized healthcare strategies.
Sequencing genomes involves mapping out the DNA sequence of an individual, which can reveal genetic predispositions to various diseases, potential responses to specific medications, and other crucial health-related information. This process begins with the extraction of DNA from a patient’s cells, followed by the use of sophisticated technologies to read the sequence of nucleotides. The resultant data is then analyzed to identify genetic variations that may influence health outcomes.
One of the most significant breakthroughs in genomic medicine is the ability to identify biomarkers that can predict the efficacy of certain treatments. For instance, in oncology, genomic profiling of tumors can reveal mutations that are targetable by specific drugs, allowing for more effective and less toxic treatment plans. Additionally, advancements in CRISPR technology have paved the way for potential gene editing therapies, offering hope for curing genetic disorders at their root cause.
The USA is home to several pioneering research projects and institutions dedicated to advancing genomic medicine. The National Institutes of Health’s All of Us Research Program aims to gather genetic data from a million participants to enhance our understanding of how genes, environment, and lifestyle contribute to health and disease. Similarly, the Precision Medicine Initiative is another ambitious project focused on developing personalized treatments based on genetic information.
The strides made in genomic medicine are not just limited to research laboratories. Clinical applications are becoming increasingly common, with genetic testing being integrated into routine healthcare to predict disease risk and guide preventive measures. As we move forward, the continued integration of genomic data into everyday medical practice holds the promise of more precise, effective, and personalized healthcare for all.
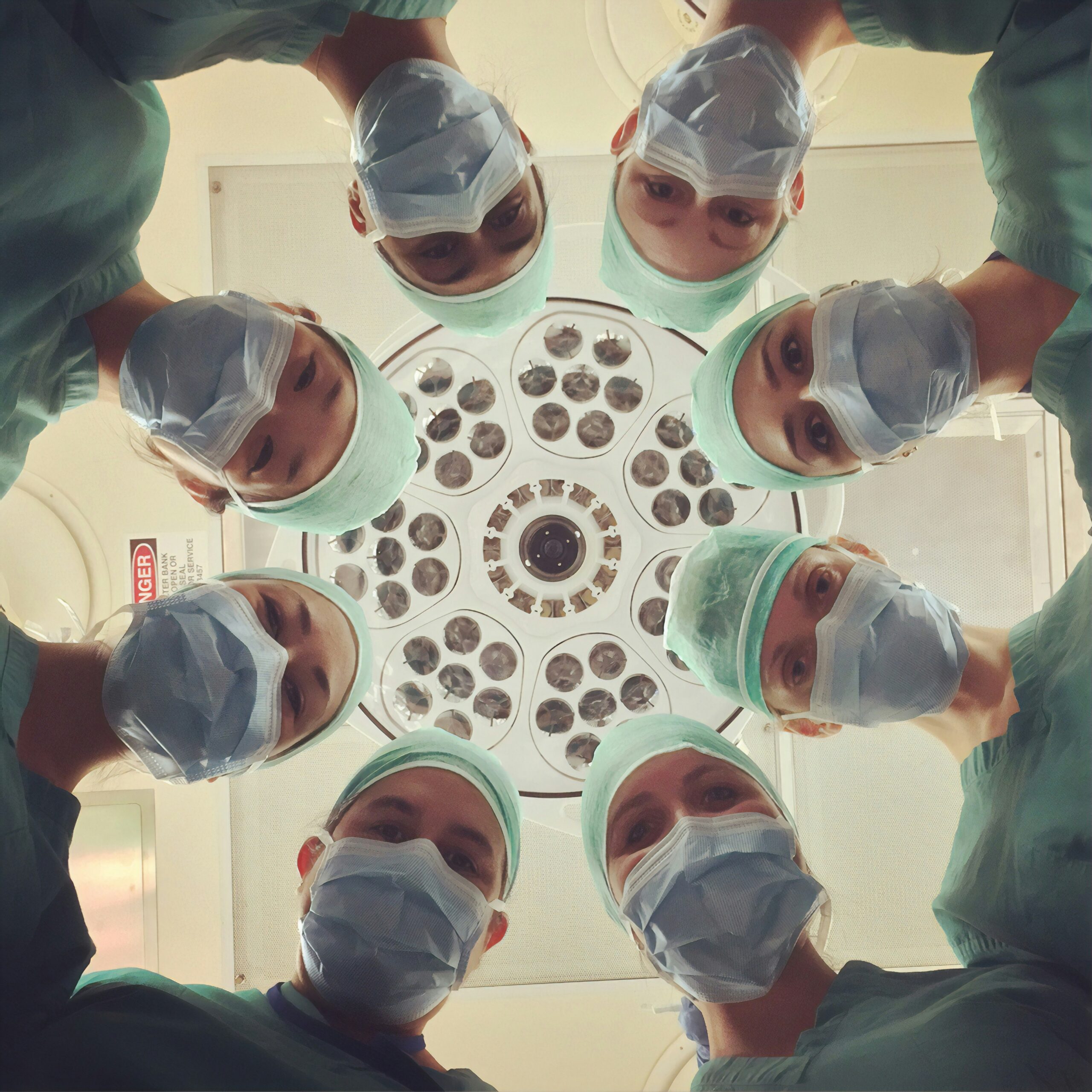
Robotics and Automation in Surgery
Robotics and automation have revolutionized the field of surgery, introducing unprecedented levels of precision and efficiency. Robotic-assisted surgery, in particular, has garnered significant attention for its potential to enhance surgical outcomes and streamline procedures. One of the most prominent examples of this innovation is the Da Vinci Surgical System, which has been widely adopted in hospitals across the United States.
The Da Vinci Surgical System exemplifies the cutting-edge advancements in robotic-assisted surgery. This sophisticated system allows surgeons to perform complex procedures with enhanced precision, flexibility, and control. By utilizing high-definition 3D vision and tiny, wristed instruments that bend and rotate far greater than the human hand, the system enables minimally invasive surgeries that significantly reduce recovery times and lower the risk of complications. Such advancements are particularly beneficial in delicate operations, such as cardiac, colorectal, and urologic surgeries, where precision is paramount.
Beyond the Da Vinci system, other robotic platforms and automation technologies are making significant strides in healthcare. For instance, robotic orthopedic surgery systems are becoming increasingly common for joint replacements and spinal surgeries. These systems use pre-operative imaging and computer algorithms to create a precise surgical plan, which the robot then executes with remarkable accuracy. This level of precision not only improves surgical outcomes but also enhances patient safety and satisfaction.
Automation in surgery extends beyond the operating room. Advanced robotics are also being utilized in pre-operative planning and post-operative care. Automated systems can assist in creating detailed surgical plans based on patient-specific data, ensuring tailored and effective treatment strategies. Additionally, robotic rehabilitation devices are aiding in faster and more efficient recovery, providing personalized therapy sessions that adapt to the patient’s progress.
In summary, the integration of robotics and automation in surgery is reshaping patient care in the United States. These technologies are not only elevating the standards of precision and safety but also paving the way for more efficient and patient-centric healthcare. The ongoing advancements in robotic-assisted surgery and automation hold promise for continued improvements in surgical outcomes and overall patient well-being.
Wearable Health Technology
The wearable health technology market has seen significant growth in recent years, particularly in the USA. This expansion encompasses a variety of devices, including fitness trackers, smartwatches, and medical-grade wearables that monitor a range of health metrics. These devices are designed to collect real-time health data, providing users with valuable insights into their physical well-being. By continuously tracking parameters such as heart rate, sleep patterns, and physical activity, wearables play a crucial role in promoting preventive care and encouraging individuals to take an active role in managing their health.
Fitness trackers and smartwatches are among the most popular categories of wearable health technology. Devices such as the Apple Watch and Fitbit have become household names, offering features like heart rate monitoring, activity tracking, and even ECG readings. These wearables not only help users stay motivated to maintain a healthy lifestyle but also provide critical data that can be shared with healthcare providers for more personalized care. By keeping tabs on daily activities and vital signs, users can identify patterns and make informed decisions about their health behaviors.
Medical-grade wearables are another essential segment within this market. Devices such as continuous glucose monitors (CGMs) for diabetes management, and wearable electrocardiogram (ECG) monitors for heart patients, offer precise and constant health tracking. These wearables provide real-time data that can alert users and healthcare professionals to potential health issues before they become critical, thereby enhancing patient care and reducing hospital visits. The integration of these devices with mobile apps and cloud-based platforms allows for seamless data sharing and remote monitoring, further enriching the patient care experience.
The impact of wearable health technology on patient care cannot be overstated. These devices empower patients by providing them with actionable health information, fostering a culture of proactive health management. As the technology continues to evolve, we can expect even more sophisticated wearables that offer greater accuracy and more comprehensive health monitoring capabilities. This ongoing innovation in wearable health technology is set to play a pivotal role in shaping the future of patient care in the USA and beyond.
Digital Health Records and Data Interoperability
The advent of digital health records, specifically Electronic Health Records (EHRs), has significantly transformed the landscape of healthcare delivery in the United States. EHRs have streamlined the process of managing patient information, enabling healthcare providers to access comprehensive patient histories promptly. This enhanced accessibility not only improves the efficiency of medical treatments but also minimizes the risk of errors, ensuring a higher standard of patient care.
One of the key benefits of EHRs is their ability to facilitate seamless data exchange between diverse healthcare providers. This interoperability ensures that critical patient information, such as medical history, allergies, and current medications, is readily available across different healthcare settings. By bridging the communication gap between primary care physicians, specialists, and hospitals, EHRs contribute to more coordinated and informed decision-making, ultimately enhancing patient outcomes.
Government initiatives have played a pivotal role in promoting data interoperability within the healthcare sector. The Office of the National Coordinator for Health Information Technology (ONC) has established various standards and regulations to encourage the adoption of interoperable health information systems. Notably, the 21st Century Cures Act mandates that healthcare providers and IT developers ensure patient data is accessible, shareable, and usable across different platforms. This legislative framework aims to eliminate information silos, fostering a more interconnected and efficient healthcare ecosystem.
Furthermore, the Trusted Exchange Framework and Common Agreement (TEFCA) is another vital initiative spearheaded by the ONC. TEFCA provides a standardized approach for nationwide health information exchange, ensuring that healthcare providers can securely and effortlessly share patient data. By fostering a collaborative environment, these initiatives strive to enhance the interoperability of health records, paving the way for innovations in patient care and clinical research.
Overall, the advancements in digital health records and data interoperability are reshaping patient care in the USA. Through the seamless exchange of information, healthcare providers can deliver more precise and timely treatments, ultimately driving better health outcomes for patients across the nation.
Future Prospects and Challenges
The landscape of healthcare innovations in the USA is poised for substantial advancements, yet it is not without its challenges. As we look to the future, the integration of cutting-edge technologies such as artificial intelligence (AI), machine learning, and telemedicine promises to revolutionize patient care. These technologies offer the potential to enhance diagnostic accuracy, personalize treatment plans, and facilitate remote consultations, thus extending the reach of quality healthcare.
However, these advancements bring forth significant challenges, particularly in the realms of data privacy and cybersecurity. With the increasing digitization of healthcare records, the protection of sensitive patient information against cyber threats becomes paramount. Ensuring robust cybersecurity measures and compliance with regulations such as the Health Insurance Portability and Accountability Act (HIPAA) will be crucial. Healthcare institutions must invest in advanced cybersecurity infrastructure to safeguard patient data and maintain trust.
Another critical challenge is the digital divide, which refers to the disparity in access to digital technologies among different population groups. Rural areas and underserved communities often face barriers to accessing high-speed internet and digital health services. Addressing this divide will require concerted efforts from both the public and private sectors. Initiatives such as expanding broadband infrastructure and offering digital literacy programs can help bridge this gap, ensuring that all individuals benefit from healthcare innovations.
Looking forward, the potential for continued innovation in the healthcare sector remains promising. Collaborative efforts among healthcare providers, technology companies, and policymakers will be essential to navigate these challenges. By fostering a culture of innovation and prioritizing patient-centric approaches, the USA can continue to lead in healthcare advancements, ultimately improving patient outcomes and shaping the future of healthcare delivery.
FinTechZoomUs Very well presented. Every quote was awesome and thanks for sharing the content. Keep sharing and keep motivating others.
Newtoki For the reason that the admin of this site is working, no uncertainty very quickly it will be renowned, due to its quality contents.